How are dietary proteins beneficial to bone health?
18 August 2020
Our physical abilities change throughout life. They gradually increase with age until their maximum between 20 and 30 years old.1 After a stagnation period, then there is a decline.2 The beginning of this stage depends on number of factors: genetic, food intake, physical activity, and the global health state.3 With age, complications may arise especially in bones. After the age of 50, it is not uncommon to see a progressive bone weakening: this is osteopenia.
Osteopenia? What is the difference between osteopenia and osteoporosis we hear about fairly regularly?
As shown in figure 1, it is possible to simplify the evolution of bone health degradation in 3 steps. Before the age of 50, mineral density is generally normal and bones are strong. Then the first complications appear: bones start to weaken and the fracture risk increase. This is osteopenia. At this point, the aim is to strengthen bone mass to delay osteoporosis as much as possible, even recover a good bone health. If nothing is done, bones will keep getting worse: this is the typical bone demineralization of osteoporosis (figure 2).4

Figure 1: Evolution of human bone health degradation from the age of 50.5
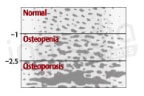
Figure 2: Bone density evaluation based on bone density score. The more this score is low, the more porous bones are.6
Do these complications concern everyone?
Yes, they do. With age, it is perfectly natural to observe a declining bone health. However, some factors can potentially increase the occurrence of this complications: sex (during their lifetime, more than half of women will on average have an osteoporotic fracture compared to only one third of men)7, exposition to certain harmful substances (alcohol, smoke), diet and physical activity.8
Is it possible to reduce the risk of bone fragility by changing your lifestyle?
Yes, you can, and we will especially focus on food. Indeed, it is well accepted that calcium and vitamin D are absolutely essential to bone health. That’s why recommended daily intake of calcium are about 1200mg/d and 10µg/j for vitamin D from the age of 50.9
However, these are not the only essential nutrients to consider. A study from « Current Osteoporosis Report » show that numbers of nutrients (figure 3) are beneficial to bone health, such as proteins.10
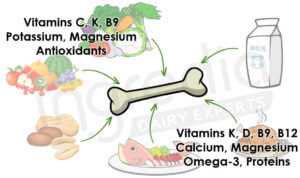
Figure 3: Nutrients acting positively on bone health.10
Can proteins be beneficial to bone health? I thought it was the opposite…
This is a common misconception. Before demonstrating their beneficial effects on bone health, it was first observed that dietary proteins cause an increase of urinary calcium. That is the reason why we firstly think that proteins could be harmful to bone health because they may generate bone demineralization.11
But this conclusion was far too hasty: even if an increase of dietary protein consumption generates an increase of urinary calcium, at the same time they enhance intestinal calcium absorption. This has been proven in 2003 study from the « American Journal of Clinical Nutrition ». As shown in figure 4, a high protein diet (2.1g/kg of body weight) allow to reach an intestinal calcium absorption of 26.3% against only 18.4% for a lower protein diet (0.7g/kg of body weight). This represents a significant increase of calcium absorption of 43%.12 13
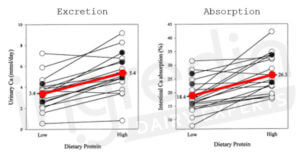
Figure 4 : Individual changes in 24h of urinary calcium and intestinal calcium absorption in response of à low- (0.7g/kg) and high- (2.1g/kg) protein diet in 20 healthy women.12 13
According to the figure 4, the high-protein diet (2.1g/kg) increase urinary calcium excretion by 2 mmol on 24h (3.4 to 5.4 mmol/d).
Knowing the calcium daily intake in the prescribed diet during the study (20 mmol/d), it is possible to deduce the amount absorbed with the low- (0.7g/kg) and the high- (2.,g/kg) protein diet: 3.7mmol with the first (18.4% of 20 mmol) and 5.3 mmol with the second one (26.3% of 20 mmol). Consequently, the high-protein diet enables to absorb 1.6 mmol more calcium in 24h.12
As a result, most of the increase in calcium excretion is explained by an increase in its intestinal absorption.
But it is not just about the calcium excretion: it is said that proteins are considered as “acidic” for the body, and this promotes bone demineralization. Is that true?
It is true that we commonly consider proteins as “acidic” for the body, in contrast to vegetables considered as “alkaline”. But the question is: does an “acidic” or “alkaline” diet have an impact on bone health? This we the topic of a 2013 review conducted by Hanly & Whiting. They summarize results from different articles and they concluded that evidences supporting the role of proteins in the development of osteoporosis are not consistent. At the same time, the authors found that a more “alkaline” diet does not appear to be particularly more beneficial for bone health.14
To summarize this review, there is no link between bone health and an “acidic” or “alkaline” diet.

Fine, but then how does proteins affect bone health? Bones are not made of protein…
And yet it is false: contrary to a common misconception, bones are not only composed of inert material: they contain proteins such as collagen.15 Like all proteins, they breakdown and regenerate perpetually: this is the protein turn-over. We studied more precisely this subject in our blog article “Why do endurance athletes need more protein?”. Consequently, a dietary protein intake increased can helps to correctly ensure this protein turn-over and maintain bone health.
But that’s not all since a 2011 review suggests that dietary proteins could act on different mechanisms of our body and thus have a positive impact on bone health: 16
- By increasing intestinal calcium absorption as we saw before.12
- By suppressing parathyroid hormone, an osteolysis hormone (bone demineralization) when its concentration is too high. The other hand, this hormone promotes bone remineralization at a low dose. So, its suppression is positive for bone health.17
- By increasing IGF-1 production, a hormone that positively contributes to bone mineralization.18
- By increasing muscular mass, providing a better bone protection and reducing fall and fracture risk. A 5-years cohort study completed in 2009 showed a positive link between muscular mass increase and bone health in elderly people.19
So, what are the best foods to maintain a good bone health?
The answer is simple: you need protein, vitamins (especially vitamin D) and minerals (calcium, magnesium, potassium) source foods. The ideal solution is to choose foods with the most complete protein, i.e. rich in essential amino acids A.
That is the reason why milk and dairy products are excellent foods that maintain bone health. As detailed in our article “How to characterize protein quality?”, dairy proteins are a good source of essential amino acids. Furthermore, minerals from the milk and especially the calcium are very bioavailable B.20 21 Finally, dairy products contain number of vitamins such as D, K, B9 and B12, which are essential for bones.22
Therefore, it is important to provide foods rich in essential nutrients for bone health for most-at-risk populations, including the elderly people. As we have seen in this article or even in precedents such as “What is the perfect protein for the elderly people?”, milk and dairy products can be a great choice to meet this demand.
For more information on our milk proteins and our expertise, contact us.
Authors: Rémi Maleterre & Audrey Boulier.
*A [Essential Amino Acids]: Amino acid that the body cannot synthesize. Therefore, they must be supplied through the diet
*B [Bioavailable]: relating to the absorption and used of a nutrient by the body. The more bioavailable a nutrient is, the more it is absorbed and used by the body.
________________________________________________________________________________________________
[1] David B. Burr, “Muscle Strength, Bone Mass, and Age-Related Bone Loss,” Journal of Bone and Mineral Research 12, no. 10 (1997): 1547–51, https://doi.org/10.1359/jbmr.1997.12.10.1547.
[2] Douglas Paddon-Jones and Blake B. Rasmussen, “Dietary Protein Recommendations and the Prevention of Sarcopenia,” Current Opinion in Clinical Nutrition and Metabolic Care 12, no. 1 (January 2009): 86–90, https://doi.org/10.1097/MCO.0b013e32831cef8b.
[3] Taylor J. Marcell, “Review Article: Sarcopenia: Causes, Consequences, and Preventions,” The Journals of Gerontology: Series A 58, no. 10 (October 1, 2003): M911–16, https://doi.org/10.1093/gerona/58.10.M911.
[4] David L. Glaser and Frederick S. Kaplan, “Osteoporosis. Definition and Clinical Presentation,” Spine 22, no. 24 Suppl (December 15, 1997): 12S-16S, https://doi.org/10.1097/00007632-199712151-00003.
[5] “Osteoporosis vs Osteopenia: Know the Difference,” OrthoAtlanta, accessed February 27, 2020, https://www.orthoatlanta.com/media/osteoporosis-vs-osteopenia-know-the-difference.
[6] Harvard Health Publishing, “Osteopenia: When You Have Weak Bones, but Not Osteoporosis,” Harvard Health, accessed February 27, 2020, https://www.health.harvard.edu/womens-health/osteopenia-when-you-have-weak-bones-but-not-osteoporosis.
[7] Philip D. Ross, “Osteoporosis: Frequency, Consequences, and Risk Factors,” Archives of Internal Medicine 156, no. 13 (July 8, 1996): 1399–1411, https://doi.org/10.1001/archinte.1996.00440120051005.
[8] Farkhondeh Pouresmaeili et al., “A Comprehensive Overview on Osteoporosis and Its Risk Factors,” Therapeutics and Clinical Risk Management 14 (November 6, 2018): 2029–49, https://doi.org/10.2147/TCRM.S138000.
[9] John A. Sunyecz, “The Use of Calcium and Vitamin D in the Management of Osteoporosis,” Therapeutics and Clinical Risk Management 4, no. 4 (August 2008): 827–36, https://doi.org/10.2147/tcrm.s3552.
[10] Shivani Sahni et al., “Dietary Approaches for Bone Health: Lessons from the Framingham Osteoporosis Study,” Current Osteoporosis Reports 13, no. 4 (August 2015): 245–55, https://doi.org/10.1007/s11914-015-0272-1.
[11] Jane E. Kerstetter and Lindsay H. Allen, “Protein Intake and Calcium Homeostasis,” in Nutrition and Osteoporosis, ed. Harold H. Draper, vol. 9, Advances in Nutritional Research (Boston, MA: Springer US, 1994), 167–81, https://doi.org/10.1007/978-1-4757-9092-4_10.
[12] Jane E. Kerstetter, Kimberly O. O’Brien, and Karl L. Insogna, “Dietary Protein, Calcium Metabolism, and Skeletal Homeostasis Revisited,” The American Journal of Clinical Nutrition 78, no. 3 (September 1, 2003): 584S-592S, https://doi.org/10.1093/ajcn/78.3.584S.
[13] J. E. Kerstetter, K. O. O’Brien, and K. L. Insogna, “Dietary Protein Affects Intestinal Calcium Absorption,” The American Journal of Clinical Nutrition 68, no. 4 (October 1998): 859–65, https://doi.org/10.1093/ajcn/68.4.859.
[14] David A. Hanley and Susan J. Whiting, “Does a High Dietary Acid Content Cause Bone Loss, and Can Bone Loss Be Prevented with an Alkaline Diet?,” Journal of Clinical Densitometry: The Official Journal of the International Society for Clinical Densitometry 16, no. 4 (December 2013): 420–25, https://doi.org/10.1016/j.jocd.2013.08.014.
[15] Bach Quang Le et al., “The Components of Bone and What They Can Teach Us about Regeneration,” Materials 11, no. 1 (December 22, 2017): 14, https://doi.org/10.3390/ma11010014.
[16] Jane E. Kerstetter, Anne M. Kenny, and Karl L. Insogna, “Dietary Protein and Skeletal Health: A Review of Recent Human Research,” Current Opinion in Lipidology 22, no. 1 (February 2011): 16–20, https://doi.org/10.1097/MOL.0b013e3283419441.
[17] G. Lombardi et al., “The Roles of Parathyroid Hormone in Bone Remodeling: Prospects for Novel Therapeutics,” Journal of Endocrinological Investigation 34, no. 7 Suppl (July 2011): 18–22.
[18] J. P. Bonjour et al., “Protein Intake and Bone Growth,” Canadian Journal of Applied Physiology = Revue Canadienne De Physiologie Appliquee 26 Suppl (2001): S153-166, https://doi.org/10.1139/h2001-050.
[19] Xingqiong Meng et al., “A 5-Year Cohort Study of the Effects of High Protein Intake on Lean Mass and BMC in Elderly Postmenopausal Women,” Journal of Bone and Mineral Research: The Official Journal of the American Society for Bone and Mineral Research 24, no. 11 (November 2009): 1827–34, https://doi.org/10.1359/jbmr.090513.
[20] Elizabeth F. Buzinaro, Renata N. Alves de Almeida, and Gláucia M. F. S. Mazeto, “[Bioavailability of dietary calcium],” Arquivos Brasileiros De Endocrinologia E Metabologia 50, no. 5 (October 2006): 852–61, https://doi.org/10.1590/s0004-27302006000500005.
[21] Léon Guéguen and Alain Pointillart, “The Bioavailability of Dietary Calcium,” Journal of the American College of Nutrition 19, no. sup2 (April 1, 2000): 119S-136S, https://doi.org/10.1080/07315724.2000.10718083.
[22] Frédéric Gaucheron, “Milk and Dairy Products: A Unique Micronutrient Combination,” Journal of the American College of Nutrition 30, no. 5 Suppl 1 (October 2011): 400S-9S, https://doi.org/10.1080/07315724.2011.10719983.