Fighting undernourishment in hospitals
21 November 2021
Undernourishment affects more than 50% of patients with cancer or Alzheimer’s disease in France. It may unfortunately worsen with therapeutic management and results in increased morbidity (i.e. amplify disease) and death.
These statistics have remained unchanged for 30 years because the assessment of the patient’s nutritional status is rarely carried out. In order to bridge these nutritional deficiencies in hospitals, it is important to provide adequate nutritional supplements.1 2
What is undernourishment?
Undernourishment corresponds to an imbalance between nutritional intake and the body’s needs. This can have important consequences, such as organs dysfunction or the loss of certain tissues, especially muscles. The first alarming symptom will be an important weight loss.2 3
When undernourishment becomes too important, then we have cachexia: a profound weakening of the body characterized by a significant loss of muscle mass, a deficient immune system, and a decrease in cognitive and physical abilities.4
Why is the number of undernourished patients so high?
There are several possible explanations for this high number of undernourished patients, particularly those with cancer.
First, it is not uncommon for cancer patients not to eat enough. Consequently, energy providings are inferior to the bodily needs. Causes can be multiple. The disease or the treatment may cause hormonal disturbances affecting hunger signals, or have an important psychological impact on the patient who can lose their appetite. 5
Secondly, almost one-third of cancers affects digestive organs (colon and rectum, liver, pancreas,…) and elimination organs (renal system, bladder). This can lead to dysfunctions in the digestive system and then malabsorption or misuse of certain nutrients.3 6
Finally, in the case of cancers, tumor consumes a lot of energy at the expense of the integrity of the body. Therefore, it is essential for the patient to consume a sufficient amount of energy and essential nutrients so as not to increase deficiencies.4 7
What are the most common nutritional deficiencies in these patients?
The first nutritional deficiency that may show visible side effects is the lack of proteins. The protein need is about 0.8g/kg of bodyweight per day.8 9
Protein deficiency exists when the subject does not consume enough proteins to meet his needs (so less than 0.8g/kg/d) or when an essential amino acidA is deficient. That is why hospitalized patients, who consume less food and/or do not assimilate them as well, are much more exposed to a lack of protein.10
The deficiency of one or more essential amino acids is also amplified if the person does not consume enough proteins of good quality and if sources are not suitably varied. For more information on the quality of proteins, see our article “How to characterize the quality of a protein”.
To synthetize muscles, our body needs all essential amino acids. This synthesis will then be proportional to the nutritional intake of the most deficient amino acid called limiting amino acid. In other words, if the requirements for the limiting amino acid are only covered up to 30%, then anabolismB will only reach 30% of its potential. As shown in Figure 1, the deficiency of a single essential amino acid is sufficient to unbalance the protein balance.11
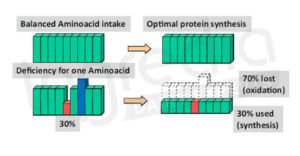
Figure 1: Effect of a lack of one essential amino acid on body protein synthesis.9
A chronic imbalance in protein intake can lead to a progressive loss of muscle mass accompanied by a decrease in physical strength.1 2 4 But this is not the only risk of muscle mass decrease. It can also lead to a gradual decrease in the proper functions of immune system due to the need of amino acids. This would lead to an increase in morbidity and risk of serious infection, and death (figure 2).12 13
Therefore, an adequate diet and especially a sufficient protein intake is vital for these patients.
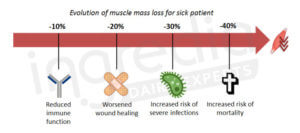
Figure 2: Impact of muscle mass loss for sick patient.12 13
Shouldn’t we consume more proteins to make sure we do not run out of amino acids?
Indeed, we often consider the value of 0.8g of proteins per kg of bodyweight per day. However, for a patient affected by a disease such as cancer, it is recommended to consume more proteins. Based on current scientific knowledge, it has been shown that a consumption of at least 1.2 to 1.6g/kg/d of high-quality proteins appears to be the ideal intake for optimal health in diseased adults.2 8 14
Furthermore, a 2009 clinical study has tried to find a link between nutrition and mortality reduction in critically ill patients. It has been shown that an increase in energy intake of an average of 1034kcal with 47g of proteins per day can significantly reduce the risk of death in undernourished patients or in important weight loss situation (figure 3).15
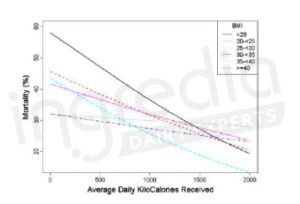
Figure 3: Relation between daily intake (including 18% of proteins) and 60-day mortality expressed with the BMI (Body Mass Index).15
Moreover, other studies have shown a strong correlation between increasing energy consumption (> 1.2 g/kg/d) and the improvement of the health status in sick patients, resulting in a mortality reduction. 7 13 16
What can be the solution to adequately meet the nutritional needs of these patients?
There are two solutions to better cover the nutritional needs of these patients.
The first one is simply to enrich the diet. The aim is then to increase the energy and protein intake without increasing the food volume too much. In order to do this, different products can be used, such as milk powder (whole milk, whey or casein), whole condensed milk, grated cheese, eggs, peanut butter, cream, oil and butter. These foods represent either a high caloric load, especially in the case of fatty foods, or a concentrate of essential nutrients, in the case of eggs and milk products. 17
Unfortunately, enriching the diet is often insufficient to meet nutritional needs of the patient, more particularly in older subjects.18 This is the reason why it is possible to consider an oral nutritional supplement. Then we bring high-calories nutritional supplements and especially rich in proteins and micronutrients (vitamins and minerals) in order to fight against malnutrition. These products are easy and fast to assimilate and can be adapted to the patient tastes: drink, dessert cream, soup, etc… The French National Authority for Health (HAS) recommends the prescription of hyper-energetic and/or hyper-protein products to achieve a dietary supplement of 400kcal/d and/or 30g of proteins per day, most often with 2 products per day.19 20
What kind of proteins is contained in these oral nutritional supplements?
These products often contain micellar caseins because they are complete proteins that can meet the nutritional needs of undernourished people. Moreover, they are ideal for the formulation of drinks or dessert creams because they are resistant to heat treatments and they allow for the conservation of the desired texture of the product.21
For more information, please contact us
Authors: Rémi Maleterre & Audrey Boulier.
*A [Essential Amino Acids]: Amino acids the body cannot synthesize. Therefore they must be supplied through the diet.
*B [Anabolism]: Muscular protein synthesis.
_________________________________________________________________________________________
[1] S. Benoist, A. Brouquet (2015). Dépistage de la dénutriton. Nutritional assessment and screening for malnutrition. Journal de Chirurgie Viscérale, 152(1):3-7. Pub February 2015. https://doi.org/10.1016/S1878-
[2] SFNEP (Société Francophone Nutrition Clinique et Métabolisme). « Nutrition chez le patient adulte atteint de cancer ». SFNEP professional recommandation [présentation of november 2012]
[3] P. Shetty (2006). Malnutrition and undernutrition. Medicine, 34(12):524-529. Pub December 2006. https://doi.org/10.1053/j.mpmed.2006.09.014
[4] J.M. Argilés (2005). Cancer-associated malnutrition. Eur J Oncol Nurs. 9(2):S39-50. https://doi.org/10.1016/j.ejon.2005.09.006
[5] Cancer Treatment Centers of America. “Malnutrition” [online] https://www.cancercenter.com/integrative-care/malnutrition. Last accessed September 3, 2019.
[6] American Cancer Society: Cancer Facts and Figures 2019. Atlanta, Ga: American Cancer Society, 2019 [online]. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/cancer-facts-and-figures-2019.pdf Last accessed September 3, 2019.
[7] H.F.R. da Cunha, E.E.M. da Rocha, M. Hissa (2013). Protein requirements, morbidity and mortality in critically ill patients: fundamentals and applications. Rev Bras Ter Intensiva, 25(1):49-55. Pub January 2013. https://doi.org/10.1590/S0103-507X2013000100010
[8] Poortmans, J.R., Carpentier, A., Pereira-Lancha, L.O., & Lancha Jr., A. (2012). Protein turnover, amino acid requirements and recommendations for athletes and active populations. Brazilian Journal of Medical and Biological Research, 45(10), 875-890. Epub June 06, 2012. https://dx.doi.org/10.1590/S0100-879X2012007500096
[9] National agency of food safety, environmend and work (ANSES). (2019) Les protéines : définition, rôle dans l’organisme, sources alimentaires. At: https://www.anses.fr/fr/content/les-prot%C3%A9ines
[10] D.W. Nixon, S.B. Heymsfield, A.E. Cohen, M.H. Kutner, J. Ansley, D.H. Lawson, D. Rudman (1980). Protein-calorie undernutrition in hospitalized cancer patients. The American Journal of Medicine, 86(5): 683-690. Pub May 1980. https://doi.org/10.1016/0002-9343(80)90254-5
[11] M.F. Holick (2003). Vitamin D: a millennium perspective. J Cell Biochem. 1;88(2):296-307. Pub February 1, 2003. https://doi.org/10.1002/jcb.10338
[12] D.W. Chang, L. DeSanti, R.H. Demling (1998). Anticatabolic and anabolic strategies in critical illness: a review of current treatment modalities. Shock, 10(3):155-60. Pub September 1998.
[13] Frebesenius Kabi. « The Role of Protein in critically ill patients » [online]. https://clinicalnutrition.com.ar/en/the-role-of-protein-in-critically-ill-patients/. Last accessed September 6, 2019.
[14] S.M. Philips, S. Chevalier, H.J. Leidy (2016). Protein « requirements » beyond the RDA : implications for optimizing health. Adv. Physiol. Nutr. Metab. 41(5): 565-572. Epub February 9, 2016. https://doi.org/10.1139/apnm-2015-0550
[15] C. Alberda, L. Gramlich, N. Jones, K. Jeejeebhoy, A.G. Day, R. Dhaliwal (2009). The relationship between nutritional intake and clinical outcomes in critically ill patients: results of international multicenter observational study. Intensive Care Medicine, 35(10):1728-1737. Pub July 02, 2009. https://doi.org/10.1007/s00134-009-1567-4
[16] P.J.M Weijs, S.N. Stapel, S.D.W. de Groot, R.H. Driessen, E. de Jong, A.R.J. Girbes, R.J.M. Strack van Schijndel, A. Beishuizen (2011). Optimal Protein and Energy Nutrition decreases mortality in mechanically ventilated, critically ill patients. Journal of Parenteral and Enteral Nutrition, 36(1):60-68. Pub December 13, 2011. https://doi.org/10.1177/0148607111415109
[17] B. Dorner (2009). Fortify to enhance nutritional value. Today’s Dietitian, 11(7):20. Pub July 2009. https://www.todaysdietitian.com/newarchives/062909p20.html
[18] C. Gaillard, E. Alix, Y. Boirie, G. Berrut, P. Ritz (2008). Are elderly hospitalized patients getting enough protein? Journal of the American Geriatrics Society. 56(6):1045-1049. Pub June 02, 2008. https://doi.org/10.1111/j.1532-54152008.01721
[19] I. Bourdel-Marchasson, M. Barateau, V. Rondeau, L. Dequae-Merchadou, N. Salles-Montaudon, J.P. Emeriau, G. Manciet, J.F. Dartiques (2000). A multi-center trial of the effects of oral nutritional supplementation in critically ill older inpatients. Nutrition, 16(1):1-5. Pub January 2000. https://doi.org/10.1016/s0899-9007(99)00227-0
[20] HAS (French National Authority for Health). « Synthèse des recommandations professionnelles (2007) ». Stratégie de prise en charge en cas de dénutrition protéino-énergétique chez la personne âgée. [online]. https://www.has-sante.fr/upload/docs/application/pdf/synthese_denutrition_personnes_agees.pdf. Last accessed September 4, 2019.
[21] Ingredia, Prodiet Fluid. The Innovative Micellar Casein dedicated to high protein beverages. [online] https://www.prodiet-fluid.com/. Last accessed September 4, 2019